
Junctional escape rhythm (C) is characterized by a narrow QRS complex rhythm with a rate of 4060 beats/minute, without association between atrial. Atrial fibrillation (A) is characterized by an irregularly irregular rhythm with a narrow QRS complex in the absence of P waves.
Varying degrees of block can appear on one recording i.e 2:1 and 3:1. Ensure to scrutinise the trace so as not to confuse flutter with fibrillation. The fixed AV block ratio, 2:1, 4:1, etc may not always present. Get your query answered 247 with Expert Advice. It occurs when the upper chambers of your heart beat too fast. The QRS presentation will normally be a narrow complex and areas of the trace will have no isoelectric baseline. Is Atrial flutter 2 1 block your major concern Solve your problem quick & easy with online consultation. Atrial flutter is a type of abnormal heart rate. Type 2 atrial flutter is less common and atrial rate can reach up to 450bpm.
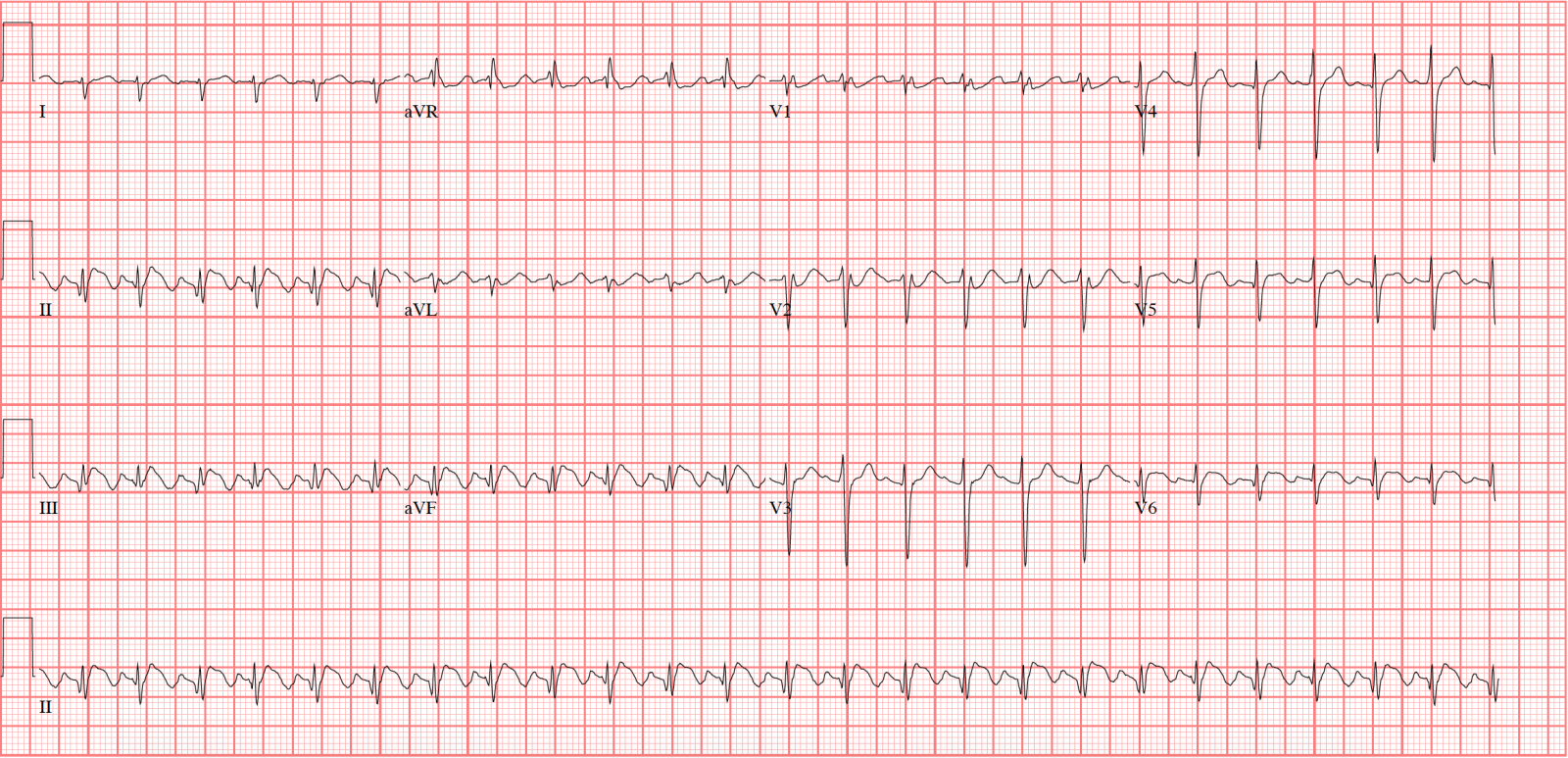
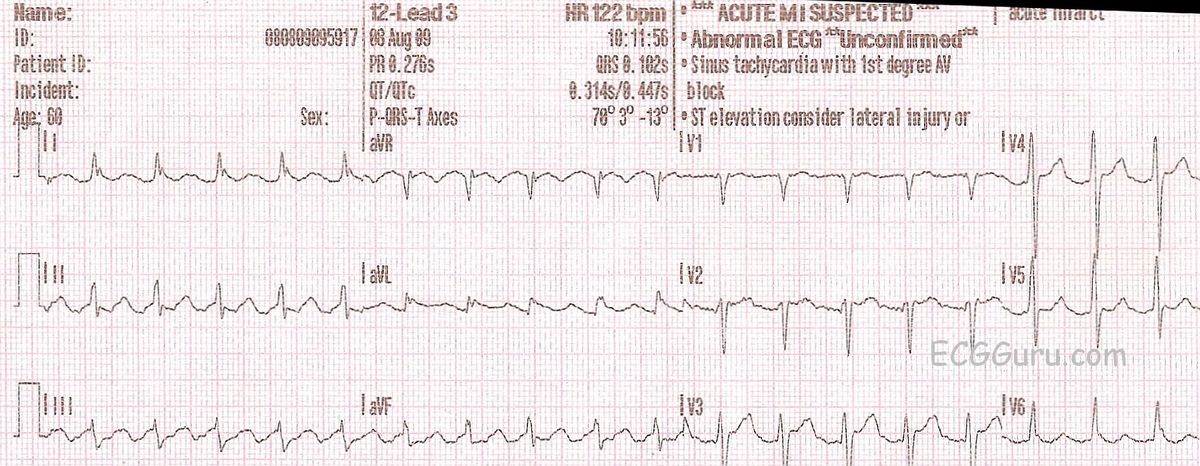
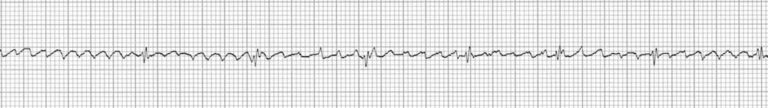
In essence, a 2:1 block implies that the ventricular rate is half that of the atrial rate, so a 4:1 rate would be a quarter.Īnti-clockwise re-entry atrial flutter accounts for around 90% of presentations and exhibits:Ĭlockwise re-entry flutter is less common, and produces: These degrees of AV block are referred to by way of a ratio of P waves and QRS complexes, the most common being 2:1 or 4:1. When interpreting this rhythm, the ratio of F waves to QRS complexes is usually included for example, atrial flutter 3:1. The rate at which the ventricles contract is dictated by the eventual atrioventricular node conduction. P waves are still present on the patient ECG, but will display a “saw-tooth” pattern know as F waves. The size of the right atrium directly corresponds to the length of the re-entry pathway, and the resulting atrial rate is somewhere between 200-400bpm, but most commonly 300. This pathway can be the result of scarring after surgery or idiopathic, so of unknown origin. In cases of atrial flutter, the normal conduction pathway of the heart from the Sinoatrial node, through the atrioventricular node to the ventricles, is interrupted causing a re-entry pathway. Recommendations for programming in order to avoid this specific form of MS failure are made accordingly and parallel algorithms for flutter detection are discussed.Atrial flutter is a supraventricular tachycardic arrhythmia that tends to occur in individuals of an advanced age, although it is linked to endurance sports, also. (B) A 2:1 atrioventricular block with slower ventricular rate and narrow QRS allows recognition of slow but typical flutter waves. Prerequisites for the ‘2:1 lock-in’ phenomenon are: (1) the sum of the AV delay and the post ventricular blanking (PVAB) must be longer than the cycle length of the atrial flutter, (2) the tachycardia detection rate must be higher than half the atrial flutter rate and (3) the maximum tracking rate (MTR) must be higher than half the atrial flutter rate. (A) Slow flutter (170 BPM) with 1:1 atrioventricular conduction and wide QRS complex (right bundle branch block and superior axis) in a patient treated with flecainide for paroxysmal atrial fibrillation.
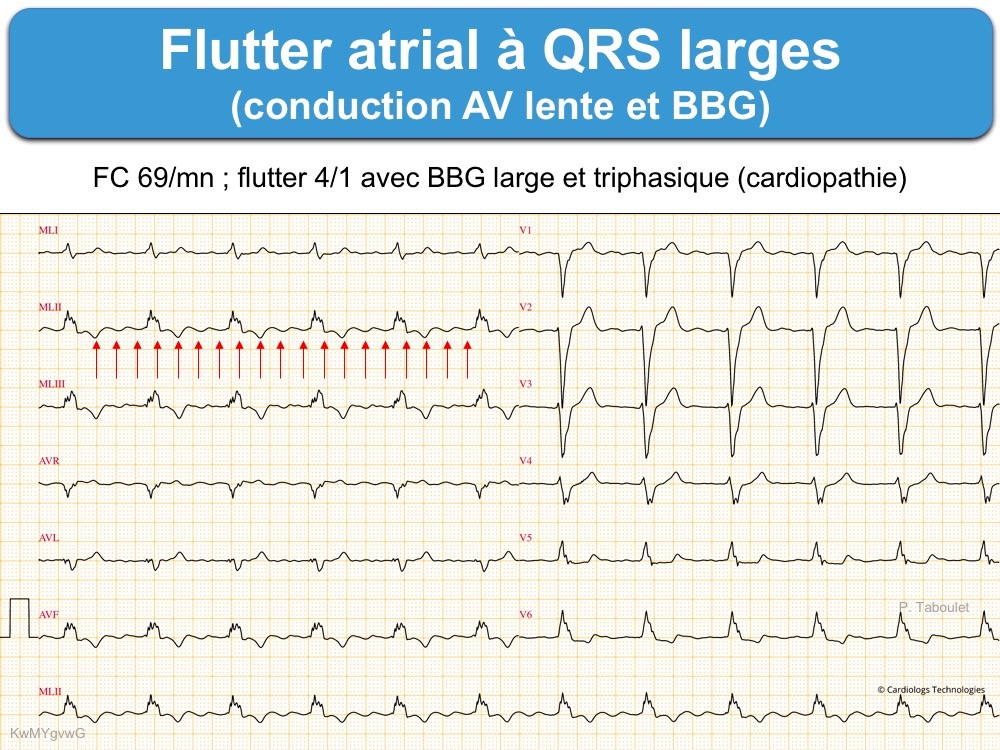
A theoretical timing model was developed to clarify the mechanism of this special form of MS failure. Since this form of MS failure implies 2:1 tracking of atrial flutter, it was coined ‘2:1 lock-in’. Seven patients (5.2%) were identified that presented with sustained rapid ventricular pacing resulting from atrial flutter with failure of automatic MS. Retrospectively the charts of 134 patients implanted with dual chamber pacemakers with MS algorithms were reviewed.


 0 kommentar(er)
0 kommentar(er)
